Introduction
Immune thrombotic thrombocytopenic purpura (iTTP) is a rare and life-threatening thrombotic microangiopathy that causes systemic platelet-rich microthrombi with multiorgan damage. Caplacizumab is an anti-von Willebrand factor humanized nano-antibody, thereby blocking platelet binding and it is the first targeted therapy approved for the treatment of iTTP, in conjunction with plasma exchange (PLEX) and immunosuppression. Two pivotal randomized controlled trials have provided positive results where the use of Caplacizumab is associated with faster platelet count recovery, decrease relapse rates significantly and reduce mortality and recurrence rates compared with placebo.
Likewise, published real-life studies support the positive results; however, today the controversy continues to exist whether Caplacizumab should be used first line or in refractory or relapsed disease.
Methods
We performed a single-center retrospective, observational analysis of clinic-biological and survival outcomes of conventional treatment alone vs addition of Caplacizumab in adult patients (≥18 years old) with confirmed diagnosis by ADAMTS13 activity of acquired iTTP (first or relapsed episode) who were treated at our institution between April 2008 and June 2023.
Baseline demographic and clinical data and laboratory values were collected at the time of diagnosis. The PLASMIC score was determined retrospectively. Day 0 was defined as the day of diagnosis as indicated by the treating physician, beginning of iTTP-specific therapy, or a reported ADAMTS13 activity measurement of less than 10%.
Time to normalization of platelet count after the start of iTTP-specific treatment was defined as the first day with a count ≥150×10 9/L (clinical response). Clinical remission, exacerbation, refractory disease, and relapse were defined according to the criteria published by Cuker et al in 2021 for the International Working Group for TTP.
Results
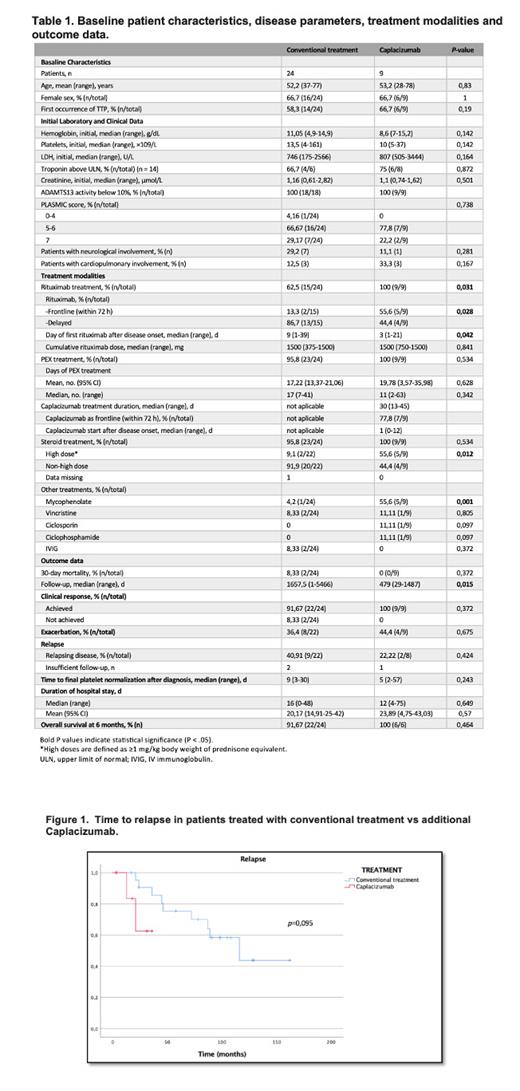
Patient characteristics, initial disease presentation, treatment modalities, individual courses, and outcome data are shown in Tables 1 and 2. Thirty-three patients were included, 24 received conventional treatment and 9 additional Caplacizumab. In 39.4% of the cases (13 of 33 episodes), iTTP was presented with a disease relapse. An initial ADAMTS13 activity of <10% was reported in all patients of Caplacizumab group (median 0%; range, 0-7%); in the conventional treatment group, in 6 patients the ADAMTS13 activity was not available at diagnosis for data consultation, in the rest of the group, ADAMTS13 activity was <10% in all cases (median 0,3%; range, 0-9%).
The median initial thrombocyte count was 12×10 9/L (range, 4-161). Troponin levels were measured in 14 patients (42,4%) at the time of diagnosis; 10 of 14 patients (71,4%) showed increased levels suggesting concomitant myocardial damage.
Due to the severity of symptoms 8 of 33 patients (24.2%), were initially treated on intensive care units. Patients were discharged from the hospital after 15 days (range, 4-75).
Thirty-two patients (96.9%) received glucocorticoids and PEX, with a median of 8 PEX treatments (range, 2-59), only one patient did not receive any treatment due to death in the first hours after hospital admission, with significant neurological and cardiac involvement. Caplacizumab treatment was started with a median of 1 day after diagnosis (range, 0-12) and the drug was used as a frontline agent in 7 of 9 patients (77.8%). Twenty-four patients (72,7%) were treated with rituximab. Ten patients received additional immunosuppressants. Platelet counts normalized to above 150×10 9/L in a median of 9 days (range, 3-30) in the conventional treatment group versus 5 days (range; 2-57) in the Caplacizumab group ( p=0.243).
Clinical remission was achieved in 31 patients. Two patients, died of iTTP complications after achieve clinical response. No differences were observed in the median time to relapse between patients treated with conventional treatment vs additional Caplacizumab (Figure 1).
Conclusions
In our experience, the use of Caplacizumab improves the clinical response rate, achieves faster platelet count recovery, and decreases relapse; another benefit is an important alleviation in the burden of care, by reducing the number of PEX sessions to achieve remission, as well as a reduction in hospital stay, although not significantly, probably limited by the number of patients included in the study.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal